If you or a loved one has been diagnosed with schizophrenia, schizoaffective disorder, or another psychotic spectrum disorder, we want you to know:
There is hope.
Our holistic, recovery-focused approach to residential treatment has helped people with schizophrenia, and related conditions achieve greater independence, maintain stronger interpersonal connections, gain more stability, and lead personally-fulfilling lives.
We can help you or your loved one, too.
Recovery is Possible
Our Approach to Healing Schizophrenia
Authored by Eric Levine, Ed.D. and Reviewed by Amy Zimmerman, DO Psychiatrist
A Focus on Wellness & Possibility
People with schizophrenia deserve to be defined by their principles and strengths. Not their illness. They deserve to live lives centered around their dreams and values. Not their symptoms.
Our residential treatment centers for schizophrenia are so much more than inpatient facilities.
The Farm (our long-term residential treatment campus) and CooperRiis at Asheville (our short-term residential treatment campus) are Healing Communities where residents receive the care they need to achieve their highest possible mental wellness and fulfillment levels.
What is schizophrenia?
Schizophrenia is a chronic mental disorder that affects how a person thinks, feels, and behaves. Its causes vary among individuals; its symptoms can include paranoia, visual and auditory hallucinations, disorganized and dysregulated thinking, difficulties with interpersonal interactions, and more.
Schizophrenia affects about one percent of the population, appearing equally in both men and women, though symptoms tend to begin earlier in men. The disorder is present in all ethnic groups. Rarely have children under the age of 16 been diagnosed with schizophrenia.
What are the different phases of schizophrenia?
The phases of schizophrenia are prodromal, active, and residual. At CooperRiis, we add the ‘recovery phase’ because rehabilitation for individuals with schizophrenia is possible.
Prodromal Phase
People with schizophrenia are often misdiagnosed in the prodromal phase because of the vast array of symptoms that can be present and their subtlety. Symptoms in the prodromal phase include:
- Withdrawal from family and social life
- A preference for being alone
- Confusion
- Outbursts of anger
- Depression
- Loss of interest in everyday activities and apathy
- Anxiety
- Odd behavior
Active Phase
Over time, symptoms of schizophrenia become evident to family and friends. During the active phase of schizophrenia, symptoms include:
- Hallucinations
- Paranoid delusions
- Disorganized speech
- Disorganized behavior
- Confusing thought patterns
- Trouble concentrating
Residual Phase
Symptoms in the residual phase of schizophrenia resemble those in the prodromal stage. While the most alarming active stage patterns have mostly subsided, low energy, listlessness, and withdrawal can still be present during this phase.
Recovery Phase
With treatment, most people who have schizophrenia will improve with time. Many of our residents come to us in the active or residual phases of schizophrenia, but no matter where they are, our goal is always the same:
To help residents move into the recovery phase by achieving the highest levels of functioning and fulfillment possible.
Can schizophrenia go away?
Currently, schizophrenia does not have a cure. However, with holistic, recovery-focused therapy and strong support networks, residents can learn how to manage their condition so they can live full, gratifying lives.
Can a person with schizophrenia live independently?
Yes, it is possible for someone with schizophrenia to live independently. Treatment focused on long-term symptom regulation and whole-person wellness can enable individuals with this condition to maintain stable employment, manage multifaceted lives, maintain relationships with others, and take care of their health.
Dream Statements
Finding Hope and Setting Realistic Goals
No matter what challenges they face, our expert staff provides residents with the dedicated, personalized support they need to overcome obstacles and take ownership of their recovery.
Resident-Centered, Relationship-Driven Care
By taking the time to get to know residents, listen to their experiences, and gain their trust, our staff members cultivate positive, nurturing relationships with residents that support them through every stage of recovery.
Education and Empowerment
Collaboration and Self-Discovery
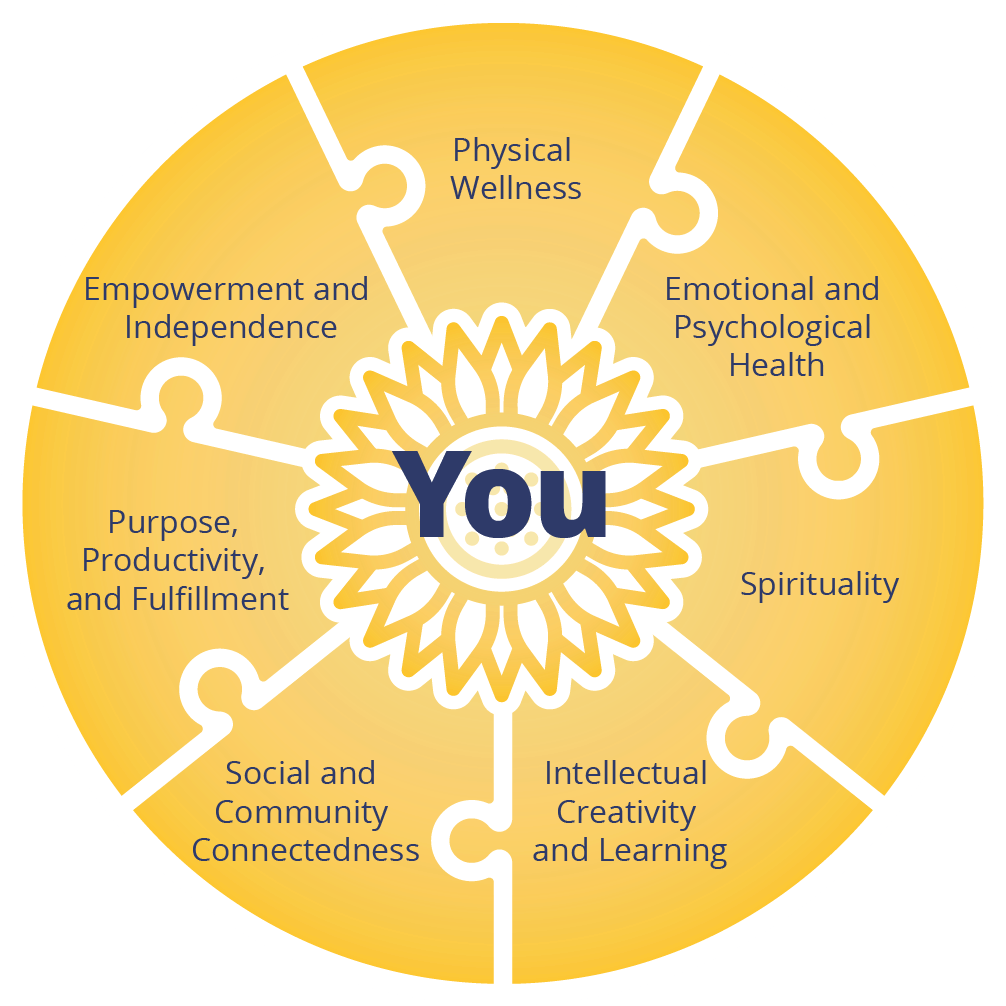
Integrated, Whole-Person Treatment
Research shows that individuals with schizophrenia respond best to multimodal recovery plans.1 That’s why, rather than rely exclusively on medications or therapy, we combine a variety of evidence-based treatments to address all of the following seven domains of health for our residents:The Seven Domains of Recovery
Treatment Plans That Meet Residents Where They Are
- Skills Training
- Social Skills Training
- Psychotherapy
- Medication
- Physical Health
- Community
- Family Education
- Housing That Feels Like Home
Skills Training
Social Skills Training
Psychotherapy
Medication Management
Physical Health
Community
Family Education
Housing That Feels Like Home
Our Recovery Model Works
Data collected over 10 years show that the residential treatment program for schizophrenia at CooperRiis works. Individuals who benefit from our holistic, recovery-focused model of care make demonstrable progress in multiple domains of health.
After participating in our program, people with schizophrenia:
- Are able to function more independently.
- Experience long-term improvements in emotional wellbeing.
- Gain stable senses of hope and purpose.
An extensive body of research and clinical experience affirms these findings: Combining psychotherapy with a strong, supportive community, structured daily routines, physical wellness programs, and an integrative approach to medication can dramatically improve the lives of those with schizophrenia.
2019 Alumni Survey Results
are engaged in either competitive employment, volunteering, or going to school.
Research Citations
1 Chien, W. T., & Yip, A. L. (2013). Current approaches to treatments for schizophrenia spectrum disorders, part I: an overview and medical treatments. Neuropsychiatric disease and treatment, 9, 1311–1332. https://doi.org/10.2147/NDT.S37485
2 Tomita, A., Lukens, E. P., & Herman, D. B. (2014). Mediation analysis of critical time intervention for persons living with serious mental illnesses: assessing the role of family relations in reducing psychiatric rehospitalization. Psychiatric rehabilitation journal, 37(1), 4–10. https://doi.org/10.1037/prj0000015