Understanding Our Approach
& Programs for Depression
For more than two decades, CooperRiis has offered residential mental health care in the Asheville area. Our depression treatment programs focus on:
A holistic approach
The recovery model of mental health care
Community and family support
Balanced independence
Person-centered therapy
Empowered living through goals and own-purpose
Why choose CooperRiis?
CooperRiis is founded on a mission to help our residents by facilitating their journey to mental health recovery through a compassionate and evidence-based approach. Here’s what sets us apart:
- Comprehensive residential and transitional care
- Family involvement
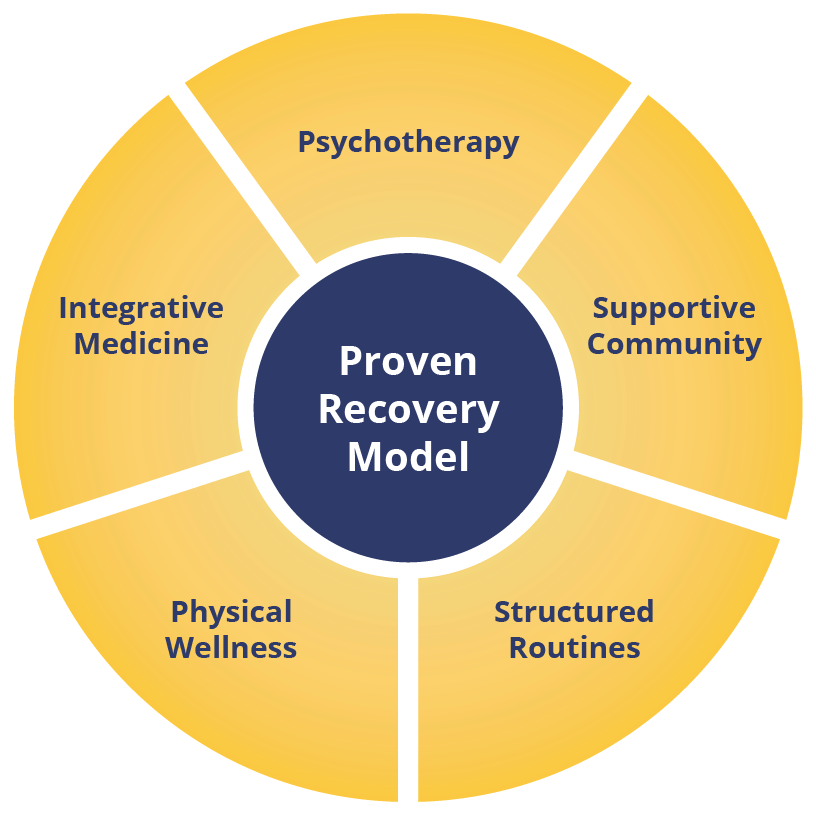
- A proven recovery model
- Flexible insurance and payment options
- Safe, vibrant, community-centered healing
- CARF accreditation
What is the Mental Health Recovery Model?
It’s a person-centered approach that empowers residents to lead self-directed lives, emphasizing holistic well-being and working towards personal goals. In comparison to the medical, or maintenance, model, the recovery model goes beyond symptom management to help participants thrive.
Who are our depression treatment programs for?
Our depression treatment programs are for adults experiencing symptoms of depression who seek:
- A person-centered, holistic recovery approach that integrates clinical care and wellness.
- A community-oriented, structured setting focused on personal growth.
- A higher level of care than outpatient services but are not in need of hospitalization.
Whether you’re new to treatment or have long managed depression, our voluntary programs provide the tools, support, and community needed to progress in your recovery work.
Who are our depression programs not for?
Our programs are not suitable for:
- Children or adolescents.
- Individuals in immediate crisis requiring hospitalization.
- Those unable to engage in a recovery-focused, communal environment.
- Persons with a history of safety concerns such as aggression, arson, or sexual offenses.
- Individuals in certain stages of dual diagnosis.
We assess each applicant to ensure a safe, supportive community and provide referrals if our programs are not the best fit.
Is this depression recovery program residential?
Yes, CooperRiis provides residential treatment for depression as part of a comprehensive recovery approach. Key features include:
- 24/7 care in a structured, supportive environment.
- A focus on self-development and healing.
- Holistic treatment integrating therapy, life skills, and meaningful activities.
- Longer stays to allow time for deeper healing and recovery.
- A therapeutic community that cultivates connection and peer support.
- Flexible entry points, including step-down care from hospitalization or step-up from outpatient treatment if needed
Residents also have access to transitional housing with outpatient programs, bridging the gap between residential care and independent living, ensuring continuity in their recovery journey.
Does CooperRiis offer inpatient level of care?
At CooperRiis, we provide compassionate residential treatment for individuals with depression, offering a supportive, home-like environment focused on healing and recovery. While residential care provides a structured setting for long-term progress, the term inpatient treatment typically refers to short-term hospitalization for acute mental health crises. If inpatient care is needed prior to joining our program, our admissions team can help guide you toward the right resources.
Where is CooperRiis located?
CooperRiis is located in Western North Carolina’s Blue Ridge Mountains. Our Asheville campus, in the historic Montford Area, features a beautiful mid-century building on four acres of rolling hills and mature trees. The Mill Spring Farm offers 94 acres with gardens, greenhouses, trails, a pond, an art barn and woodshop, plus tennis, basketball, and pickleball courts.
What is your approach at CooperRiis?
At CooperRiis, we use a unique recovery model that integrates mind and heart to help residents achieve fulfillment and independence. Residents at CooperRiis benefit from:
- Personalized dream statement: Residents create a roadmap of their hopes and goals, focusing on wellness and possibility.
- Healing community: Residents connect by sharing work, meals, and activities together.
- Holistic care: The program integrates therapies, wellness practices, diet, exercise, and self-esteem building.
- Individualized support: A resident-to-staff ratio better than 1:1 ensures personalized attention.
This compassionate, structured approach supports residents in their journey toward their best health and most meaningful living.
Does CooperRiis take insurance?
CooperRiis accepts Aetna, Cigna, and Blue Cross Blue Shield of North Carolina for in-network coverage for our Asheville program. We also submit to out-of-network insurance providers for both the Asheville and Farm programs. Transitional housing is private pay. Visit our Insurance and Fees page for more details.
What is the cost of your residential depression treatment program?
Costs vary by program. The Asheville residential program is $950 per day, while The Farm is $26,000 per month with potential rate reductions starting in the third month. Transitional housing through our Asheville Community Program is $12,500 per month for the higher level of support and $4000 per month for lower support needs. Learn more on our Insurance and Fees page.
What depression programs do you offer?
CooperRiis offers programs tailored to support recovery from depression, emphasizing holistic care and personal growth:
- Therapeutic healing farm: A residential program combining evidence-based therapies with farm activities like gardening and animal care to foster resilience and connection.
- Short-term residential program: Clinically intensive care in Asheville for shorter stays, focusing on psychotherapy, psychiatry, and wellness services in a restorative setting.
- Transitional living: Supports independence with ongoing therapy and real-world skill building.
Each program incorporates holistic approaches like mindfulness, nutrition, fitness, and life skills training to promote long-term recovery and help individuals reclaim their lives.
How long do the treatment programs for depression last?
Each person’s journey is unique, and length of stay depends on their individual goals and readiness for independent living. In general, typical stays are as follows:
- Asheville program: 45–90 days
- Farm program: 3–6 months
- Transitional living: 6–12 months
Recovery is Possible
What to Expect with CooperRiis’ Care
We believe passionately in a model that centers each resident in their own healing and recovery, which means every single person’s journey here is unique. There are some methods and features, however, which are foundational to the compassionate and effective care we deliver as part of our mental health recovery programs.
A Healing Environment
Exercise & Nutrition
Integrative Medication Approach
Compassionate Communication
Mindfulness Practices
Therapeutic Approaches
Motivational Interviewing
Family Education
Learn More About Depression
Authored by Eric Levine, Ed.D. and Reviewed by Amy Zimmerman, DO Psychiatrist
What is major depression?
Depression is a mental health condition often associated with persistent sadness, hopelessness, and a loss of interest in daily activities. Emerging research points to neurobiological differences that affect brain function and mood regulation. These differences can influence energy levels, sleep, concentration, and appetite. Up to 26% of U.S. women and 12% of U.S. men experience at least one incidence of depression in their lifetimes.
What kinds of depressive disorders are there?
Depressive disorders are categorized based on their cause, duration, and symptoms. Some types are linked to specific events or biological changes, while others, like major depressive disorder, appear to occur independently. Understanding these distinctions helps guide effective treatment. The common types of depression are:
- Major depressive disorder: A severe form of depression characterized by persistent, overwhelming sadness or hopelessness lasting at least two weeks. MDD is not tied to specific external events.
- Bipolar disorder: Characterized by swings between depressive and manic episodes, bipolar’s depressive phases include symptoms very similar to those of other depressive disorders.
- Seasonal affective disorder (SAD): Occurs most often in the winter months when there is less sunlight, typically going away in the spring and summer.
- Persistent depressive disorder: Depression that lasts for two years or longer.
- Psychotic depression: Depression accompanied by psychotic symptoms such as hallucinations, delusions, and paranoia.
- Postpartum depression: Depression that develops in the weeks or months after childbirth.
- Premenstrual dysphoric disorder (PMDD): A severe form of premenstrual syndrome, PMDD includes mood swings, fatigue, anxiety, and other disruptive symptoms.
- Situational depression: A short-term, typically stress-related type of depression. Common events that can trigger situational depression include the death of a loved one, divorce, and illness.
What are the signs and symptoms of depression?
Depression can present differently for each individual, but common symptoms include:
- Persistent sadness, irritability, or feelings of emptiness.
- Loss of interest in once-enjoyed activities.
- Significant weight changes (loss or gain).
- Changes in sleep patterns—difficulty sleeping, insomnia, or excessive sleep.
- Restlessness or agitation.
- Fatigue or loss of energy.
- Feelings of worthlessness or guilt.
- Difficulty concentrating or making decisions.
- Social withdrawal or isolation.
- Negative thinking or difficulty seeing positive outcomes.
- Thoughts of death or suicide.
How do you recover from depression?
A holistic, cross-disciplinary approach to recovery that includes psychotherapy, medication, and physical activity has been shown to be the most effective method of treating depression in adults. If you are interested in learning more about whether our residential depression recovery program is right for you or your loved one, visit our admissions page to start a conversation.
Additional Resources for Understanding Depression
Below, we’ve included some resources to help you and your family contextualize and gain new understanding around depression.
Our Recovery Model Works
An extensive body of research and clinical experience affirms these findings:
Combining psychotherapy with a strong, supportive community, structured daily routines, physical wellness programs, and an integrative approach to medication can dramatically improve the lives of those with depression.
Data collected over 10 years show that the residential treatment program for depression at CooperRiis works. Individuals who benefit from our holistic, recovery-focused model of care make demonstrable progress in multiple domains of health:





Where Respect Meets Recovery
Research Citations
1Firth J, Gangwisch J E, Borsini A, Wootton R E, Mayer E A. Food and mood: how do diet and nutrition affect mental wellbeing? BMJ 2020; 369 :m2382 https://doi.org/10.1136/bmj.m2382
2Tomita, A., Lukens, E. P., & Herman, D. B. (2014). Mediation analysis of critical time intervention for persons living with serious mental illnesses: Assessing the role of family relations in reducing psychiatric rehospitalization. Psychiatric Rehabilitation Journal, 37(1), 4–10. https://doi.org/10.1037/prj0000015