If you or a loved one has been diagnosed with post-traumatic stress disorder (PTSD), we want you to know:
There is hope.
Our whole-person, sustainable approach to recovery has helped adults aged 18+ with PTSD achieve emotional stability, build self-efficacy, and regain agency in their lives.
We can help you or your loved one too.
Recovery is Possible
Our Approach to Healing PTSD
Authored by Eric Levine, Ed.D. and Reviewed by Amy Zimmerman, DO Psychiatrist
A Focus on Wellness & Possibility
PTSD traps people in the worst moments of their lives. We recognize how painful and debilitating this is, so we meet every individual who enters our residential rehab programs at both The Farm (our long-term residential treatment center) and CooperRiis at Asheville (our short-term residential treatment center) with profound compassion.
We also believe that individuals with PTSD are capable of recovering and achieving personal fulfillment. That’s why we do more than temporarily mitigate symptoms: We provide residents the tailored, whole-person care they need to reprogram their nervous systems, reclaim control of their behaviors, and free their minds from the mire of near-constant distress.
What is PTSD?
PTSD stands for Post-Traumatic Stress Disorder. It’s an anxiety disorder that develops after experiencing/ witnessing a traumatic event firsthand or learning that a traumatic event has happened to a loved one. PTSD is often associated with veterans and wartime involvement, but many experiences can cause PTSD. Some examples are:
- Threat of death or serious injury
- Sexual abuse, violence, and rape
- Chronic physical abuse, severe emotional abuse, and neglect
- Living through natural disasters such as earthquakes, hurricanes, floods, or fires
- Community violence like attacks at a local school
- The suicide of a friend or family member
When someone experiences trauma, it’s normal for their body to enter what is often referred to as “fight-flight-or-freeze” mode. In this state, adrenaline courses, the heart pounds, muscles tense, breathing rates skyrocket, and dissociation may occur (dissociation refers to the sensation of watching yourself from above or detaching yourself from the present/reality), among other effects.
Once a traumatic event has passed, an individual’s body should eventually “downshift” from this heightened state back to normalcy. Depending on many factors, including the intensity of the event, this can take some time. However, if the body does not “come down” long after the distressing event triggering it has passed, PTSD develops.
There is still a lot of research to be done on the physiological underpinnings of PTSD, but what scientists do know is this: When an event is so traumatic that an individual’s stress hormones remain spiked for an extended period of time, there are changes in the brain that correlate with PTSD symptoms. These changes include a loss of volume in the ventromedial prefrontal cortex (vmPFC), a loss of volume in the hippocampus, and an increase in the amygdala volume.
A loss in vmPFC volume is linked to difficulties with behavioral inhibition, a loss in hippocampal volume is linked to difficulties discerning what is presently occurring and what has occurred in the past, and an increase in the size of one’s amygdala is linked to emotional regulation challenges. These issues create a debilitating constellation of symptoms that make someone feel and behave as if they are constantly in serious danger.
The good news is that all of these physiological changes and the cognitive/ behavioral symptoms that go with them can be treated and healed. Recovery from PTSD is possible, and if you’re interested in speaking with one of our friendly admissions team members about our holistic, integrative approach to healing PTSD, give us a call today.
What are the signs and symptoms of PTSD?
There are four different types of symptoms associated with PTSD:
Re-experiencing symptoms include:
- Flashbacks
- Anxiety attacks
- Nightmares
- Frightening intrusive thoughts
Avoidance symptoms include:
- Staying away from places, events, or objects that may trigger thoughts of a traumatic experience
- Avoiding thoughts or feelings related to the traumatic event
- Avoiding others
Arousal and reactivity symptoms include:
- Being easily startled
- Feeling tense or “on edge”
- Hypervigilance
- Having difficulty sleeping/ insomnia
- Angry outbursts
Cognition and mood symptoms include:
- Trouble remembering key features of a traumatic event
- Negative thoughts about oneself or the world
- Distorted feelings like guilt or blame
- Loss of interest in formerly enjoyable activities/ emotional numbness
- Episodes of dissociation, especially depersonalization (a feeling of detachment from oneself/ watching oneself from above, etc.) and derealization (a feeling of being detached from your surroundings or as if you are in a dream)
To be diagnosed with PTSD, an individual must have experienced at least one symptom from each category for at least one month and to such a severe degree that their ability to work/ relationships are impacted.
Symptoms do not always appear immediately after a traumatic experience. It can take months or even years for PTSD symptoms to manifest. What’s more, it is not unusual for someone with PTSD to experience it alongside another mental health condition, such as another anxiety disorder or depression. The prevalence of substance abuse disorders among those with PTSD is very high: According to the National Center for PTSD, 46.4% of individuals with PTSD also develop a dependency on drugs or alcohol.1
Who can get PTSD?
Anyone who experiences a significantly traumatic event can develop PTSD. Women are twice as likely as men to develop PTSD because they are at higher risk of experiencing traumas such as sexual assault or child sexual abuse.
How do you treat PTSD?
PTSD is most effectively treated with a combination of medication, therapy, and community-based interventions. When this combination of treatments is tailored to suit an individual’s specific needs and delivered by a team of experts, people can recover from this condition and go on to lead full, gratifying lives.
Call us today to speak to one of our friendly admissions staff members about how CooperRiis heals the physiological, cognitive, and behavioral components of PTSD through integrated, holistic residential care.
Dream Statements
Taking Gradual Steps Towards Manageable Goals
It can be hard for residents with PTSD to envision uplifting possibilities for their futures when they're constantly operating in survival mode. That's why our expert staff offers the personalized support residents need to safely process the trauma they've experienced, skillfully regulate their emotions, and develop new, adaptive relationships with their thoughts.
As residents engage in our Trauma Resource Model (TRM)-informed treatments, we help them reconnect with their core values and interests. This allows them not only to set personally meaningful goals, but also to take manageable steps towards them.
Holistic, Relationship-Driven Care
The success of our approach to healing PTSD hinges on the relationships we build with our residents. By taking the time to listen to their experiences, understand their values, and gain their trust, our staff creates a healing space where individuals with this condition feel safe to make progress through every stage of recovery.
Empowering Minds
Building Community
Integrated, Whole-Person Treatment
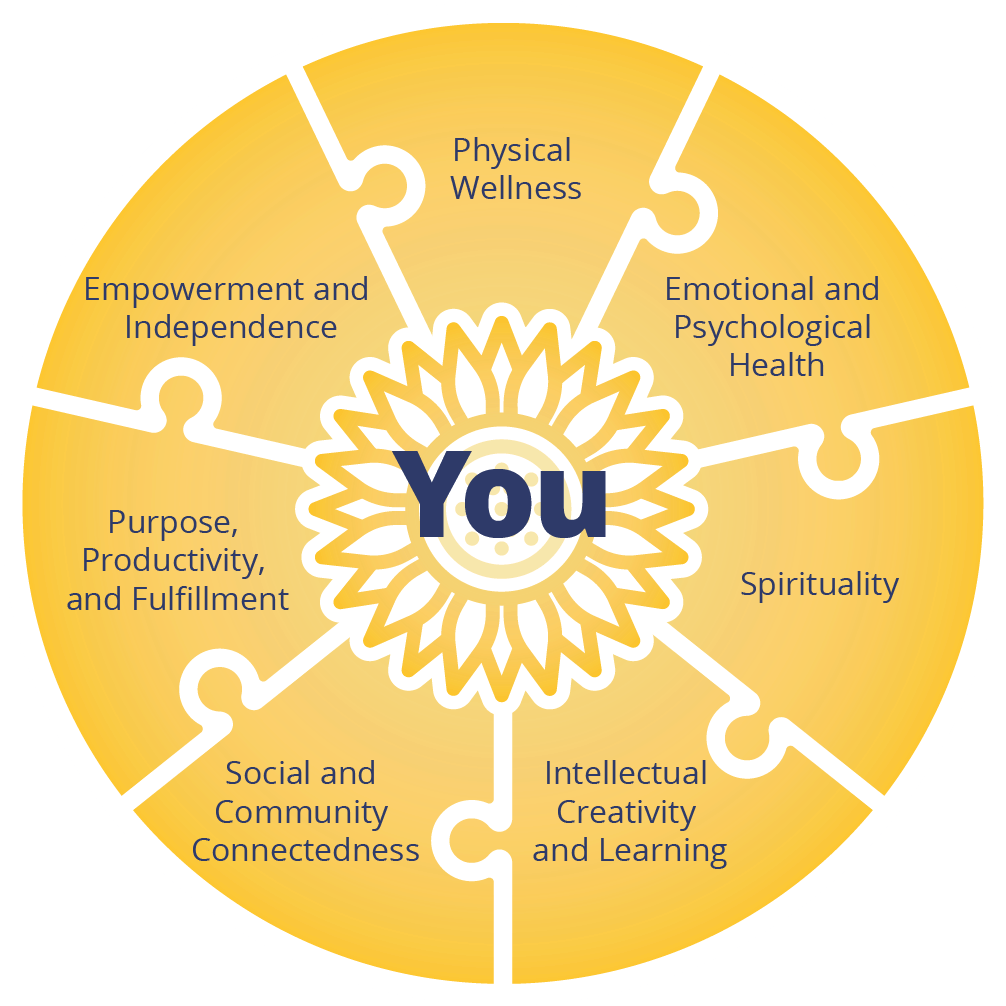
Individuals with PTSD respond best to multimodal, multi-phase treatment plans. That’s why, rather than relying exclusively on medications or therapy, we combine a variety of evidence-based treatments to address all of the following seven domains of health for our residents:
The Seven Domains of Recovery
Treatment Plans That Meet Residents Where They Are
No matter where they are on their recovery journey, every CooperRiis resident receives personalized care that allows them to make sustainable progress towards their goals. While this means every individual’s recovery plan is unique, the following types of PTSD treatments have been especially beneficial for our residents:
Soothing, Stress-Free Environment
Exercise/Movement Practices
Nutrition and Supplements
Medication
Breathwork and Mindfulness Practices
Cognitive Therapy
EMDR
WRAP Groups
Community
Family Education
Our Recovery Model Works
Data collected over 10 years show that the residential treatment program for PTSD at CooperRiis works. Individuals who benefit from our holistic, recovery-focused model of care make demonstrable progress in multiple domains of health.
After participating in our program, people with PTSD:
- Are able to carry out day-to-day functions successfully and with greater ease.
- Experience long-term improvements in emotional wellbeing.
- Gain stable senses of self-efficacy.
- Are empowered to become stewards of their own health.
An extensive body of research and clinical experience affirms these findings: Combining psychotherapy with a strong, supportive community, structured daily routines, physical wellness programs, and an integrative approach to medication can dramatically improve the lives of individuals with PTSD.
2019 Alumni Survey Results
are engaged in either competitive employment, volunteering, or going to school.
Research Citations
1https://www.ptsd.va.gov/professional/treat/cooccurring/tx_sud_va.asp
2 Tomita, A., Lukens, E. P., & Herman, D. B. (2014). Mediation analysis of critical time intervention for persons living with serious mental illnesses: Assessing the role of family relations in reducing psychiatric rehospitalization. Psychiatric Rehabilitation Journal, 37(1), 4–10. https://doi.org/10.1037/prj0000015